New Hampshire Latino News produces and amplifies stories focused on the responses to the social determinants of health. A key social determinant, Health Access & Quality is defined as the extent to which people have equitable, affordable and available access to needed healthcare services. This definition includes both physical accessibility and availability via financial means, transportation options, and other factors.
The federal government announced at the end of 2022 that it will be ending continuous Medicaid enrollment. For over 72,800 Granite Staters, that means their coverage will be gone if they don’t contact the Department of Health and Human Services (DHHS) by March 31.
This continuous enrollment, a provision of the Families First Coronavirus Response Act, allowed millions of Americans to remain on Medicaid without having to show that they still qualify. Starting April 1, the DHHS will return to its annual redetermination process, in which recipients will have to prove their eligibility for the first time since before the Covid-19 pandemic.
With the March 31 redetermination deadline rapidly approaching, the department is sending out yellow letters to New Hampshire residents that need to complete this process. State Medicaid Director Henry Lipman said that NH EASY users may receive an electronic copy of the letter as well.
The letters state in bold, “Continuous Medicaid coverage is ending,” and include instructions and resources to navigate redetermination.
“It’s going to be important for Medicaid beneficiaries to watch their mail, email and text messages for notices from the state and to complete their Medicaid renewals in order to avoid a gap in their health coverage,” said D.J. Bettencourt, deputy insurance commissioner of New Hampshire.
The over 72,000 recipients that haven’t yet completed this process ahead of March 31 will lose their Medicaid coverage if they don’t meet this deadline. That’s why Lipman said it’s important for recipients to look out for these yellow notices.
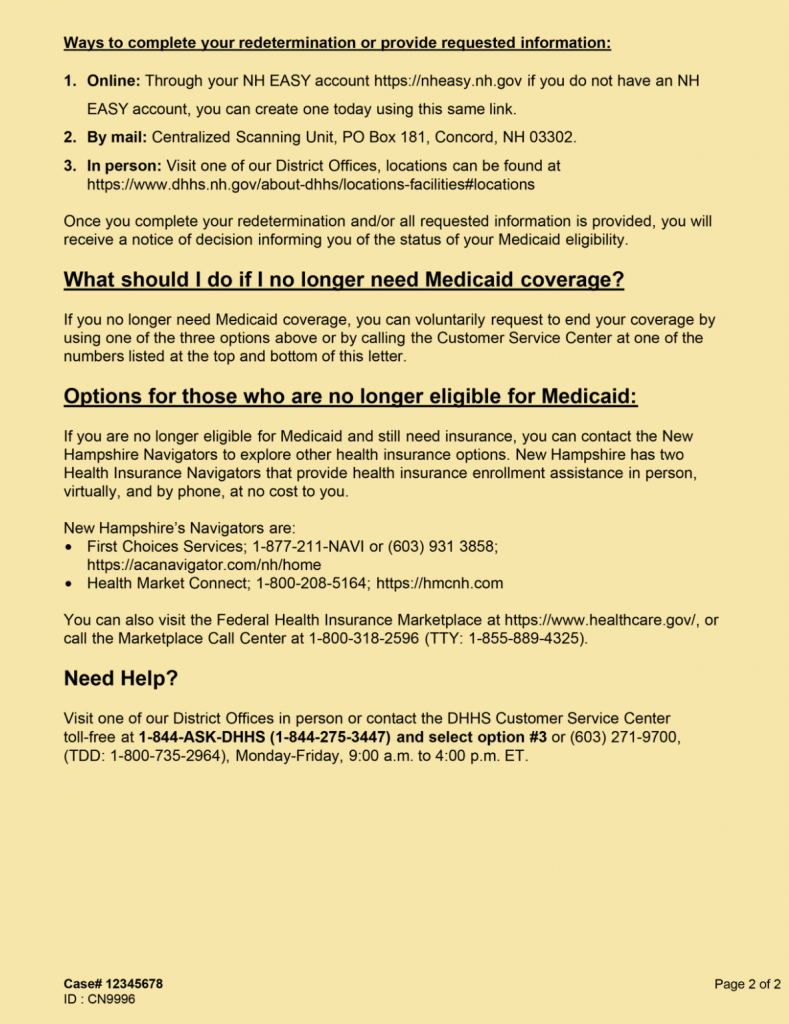
“All of the notices related to eligibility, everything now going forward is yellow during this unwind period,” he said.
Lipman said his department has been mindful of New Hampshire’s Latino and Spanish-speaking communities when coordinating this outreach campaign. Between eight and nine percent of New Hampshire Medicaid recipients are Hispanic. That’s much lower than the national average, but still a point of emphasis for Lipman and his team.
“We don’t have the necessary ethnicity data to send it out directly [to the households that need it], but we’ve made the letter available and prominent on our website in Spanish,” he said. “We’ve worked in the past with New Hampshire Public Radio and their Spanish news component. We do try to have sensitivity not only to people who speak Spanish, but to other languages.”
In preparation for an expected wave of last-minute redetermination requests, Lipman said the department increased call center capacity so recipients can have the chance to qualify.
But not everyone who completes redetermination on time will be able to keep their existing Medicaid coverage. In fact, many won’t qualify to stay on Medicaid and will have to seek out alternative health insurance options.
To help with the search, New Hampshire’s DHHS recognizes two services as the state’s Health Insurance Navigators: First Choices Services and Health Market Connect, both of which offer services in English and Spanish.
“Our goal is to find, connect with and enroll as many New Hampshire residents in whatever qualifying plan that they’re eligible for,” said Eli Cohn, navigator with Health Market Connect. “So if they’re continuing to be eligible for Medicaid, we want to keep them on Medicaid… if not, we want to get them on a healthcare plan on heathcare.gov.”
Cohn expects to be helping many state residents whose incomes are now too high to stay qualified for Medicaid.
“If they need to transition out of Medicaid because they’re over income, we can get them into a Marketplace plan that’ll still offer them some financial support,” he said.
Cohn said that Health Market Connect hasn’t gotten a lot of calls just yet about the March 31 redetermination, specifically. He anticipates that will change in the near future as recipients start reacting to the letters.
“I think it’s going to pick up really, really soon,” he said. “It feels, to a lot of people, this yellow letter looks a little threatening… A lot of the job is going to be emotional sensitivity, helping people find the peace of mind that they’re looking for by getting themselves covered.”
Benefits will end gradually for those who no longer qualify, however. Lipman said that they will remain usable for one year after a person has been ruled no longer eligible.
Additionally, the state will leave children, people in long-term care settings and other vulnerable individuals to be evaluated towards the end of this Medicaid unwind, a process expected to take about one year. This way, these groups have more time to seek alternative healthcare options, if necessary.
Resources:
First Choice Services; 1-877-211-NAVI or (603) 931 3858; https://acanavigator/com/nh/home
Health Market Connect; 1-800-208-5164; https://hmcnh.com
Federal Health Insurance Marketplace; https://www.healthcare.gov
Marketplace Call Center; 1-800-318-2596 (TTY: 1-855-889-4325)
____________________________________________________________________________
Cover photo: TaxRebate.org.uk




