A study released June 22 deemed New Hampshire as the third best performing state in healthcare in the nation, ranking top 10 nationally in almost each category. It earned the number one spot overall in Prevention and Treatment.
The 2023 Scorecard on State Health System Performance was this year’s version of an annual data assessment by The Commonwealth Fund aiming to determine how well the healthcare system is working in each state. The scorecard measured 58 areas of health access, quality, use of services, costs, health disparities, reproductive care and health outcomes to calculate the scores.
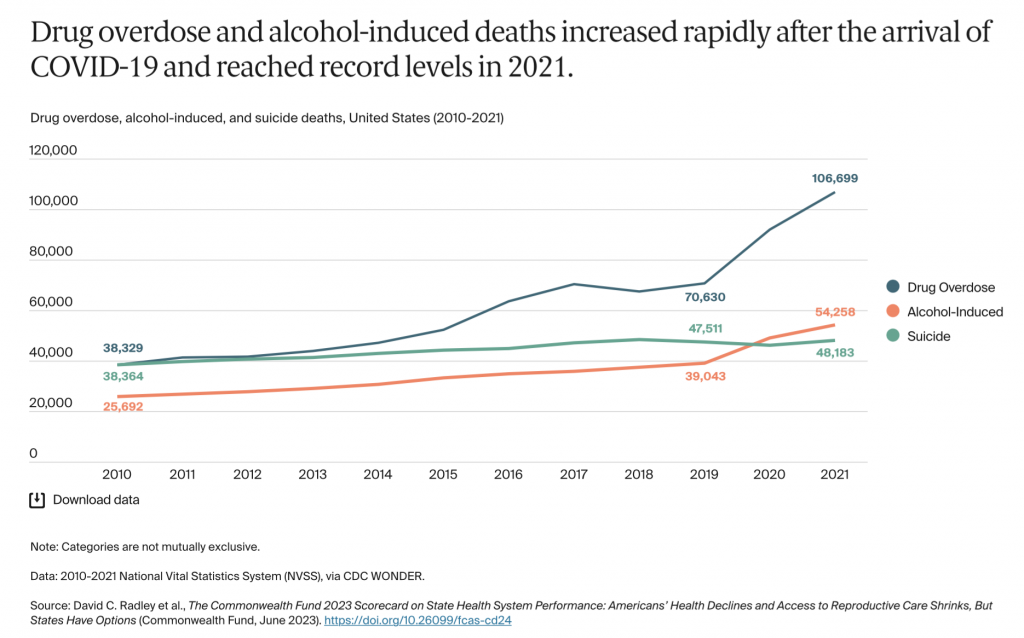
Given the effects of the pandemic the number of preventable deaths rose, but COVID-19 was not the only contributing factor. Drug and alcohol-related deaths skyrocketed as the pandemic hit. In 2021 alone, 106,699 overdoses resulted in deaths nationally, jumping from 70,630 before the pandemic began in 2019.
Temporary policies implemented during the pandemic, like continuous medicaid coverage, drove uninsurance rate to all time lows but the report also highlighted coverage gaps and inadequate insurance as issues fueling medical debt.
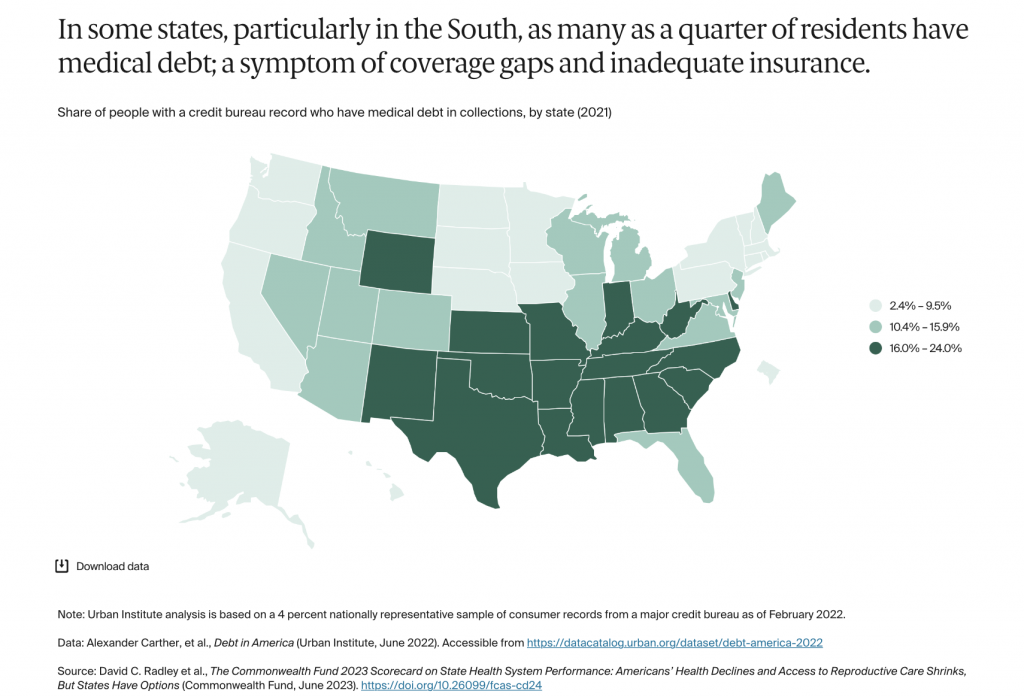
While only 6% of New Hampshiners had medical debt in collections, the national average was 13%. Comparatively, West Virginia had the highest percentage at 24%.
“While these numbers are striking, they also underestimate the real scope of the affordability crisis since they do not include debt people owe directly to hospitals or other providers,” explained Jesse Baumgartner, co-author of the report and Senior Research Associate, The Commonwealth Fund.
New Hampshire, Massachusetts, and Rhode Island were ranked the top performing states on reproductive care and women’s health.
This is the first time this category was included in the report, but the data regarding reproductive health was collected before the Dobbs decision overturned the constitutional right to abortion. Many of the states with the worst reproductive and women’s health outcomes are currently implementing harsher restrictions on this type of care.
“This really raises concerns about inequity in access and inequity in health outcomes so as we think about women’s ability to access healthcare, we have to promote policies and innovative payment models and digital tools that can really support the continuum of reproductive and women’s health care,” said co-author Laurie Zephyrin, Senior Vice President of Advancing Health Equity at The Commonwealth Fund.
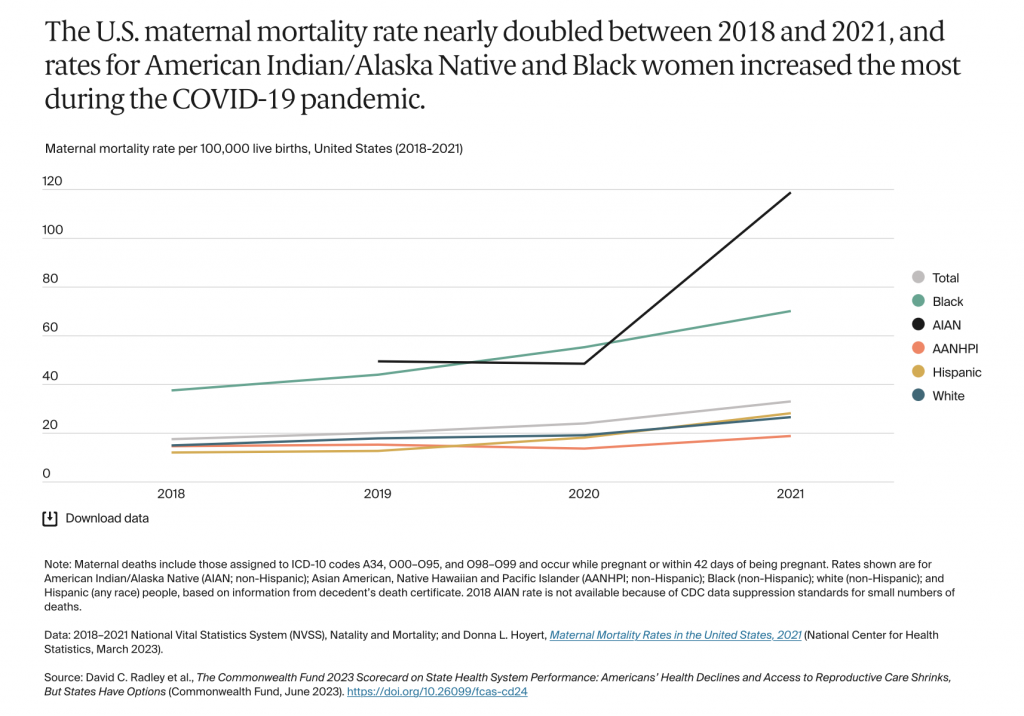
According to the report, the maternal mortality rate nearly doubled between 2018 and 2021. In 2021, the death rate for Hispanics while pregnant or within 42 days of being pregnant was 28 per 100,000 live births. American Indian and Alaskan Native women had the highest maternal mortality rate at almost 119 per 100,000 live births.
“Ultimately part of this work is to highlight where do states stand now, where do they compare to each other and really allow us to raise the alarm and say we really have to have policy interventions now to intervene before we see things worsen in the future,” said Zephyrin.